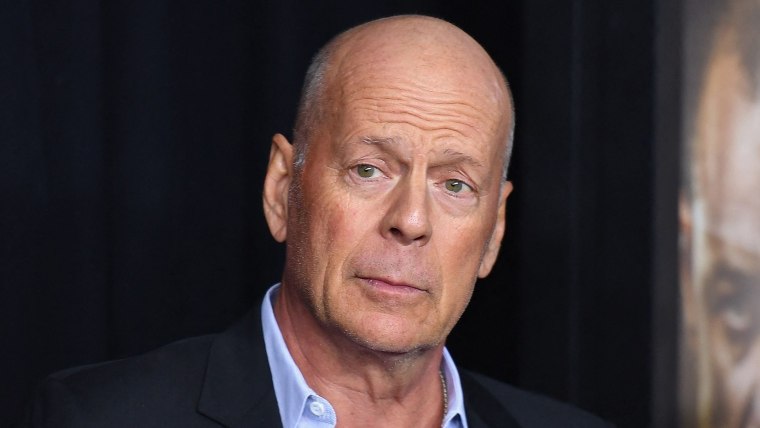
Bruce Willis' frontotemporal dementia diagnosis reveals an uncomfortable truth
Americans would prefer to not think about what happens if our minds and bodies start to decline. Caregivers don’t have that luxury.

Original article appeared here.
Last week Bruce Willis’ family announced he had been diagnosed with frontotemporal dementia. The actor had been struggling with aphasia since at least last spring. Obviously, this was not the life — a loss of independence, and a sense of self — that any of us would wish for ourselves or our loved ones. But for the many family, friends and neighbors who step up as informal caregivers for older adults across the country, Willis’ diagnosis is a reminder of a pervasive, albeit often hidden burden shouldered by millions of Americans.
Currently, more than 6.2 million individuals in the U.S. live with some form of dementia. These millions of Americans will all, slowly and over time, become progressively unable to perform even the simplest of tasks on their own. They will all eventually require care from others.
In this country, more than 80% of individuals with dementia receive care at home, which is provided by the more than 26 million informal caregivers. Without a doubt, a diagnosis of dementia is devastating for the individual, but we cannot lose sight of the profound and complex ways in which it touches the lives of those expected to provide care.
Caregivers are confronted with the difficulties of learning how to give care to a loved one, which entials managing symptoms, navigating the complexities of the health care system, finding resources and taking care of themselves too. Some might think the easy answer is to hire in-home assistance. But while some families — like Willis’ — are resource-blessed, the vast majority are not.
And dementia does not discriminate.
What is frontotemporal dementia?
For those lacking adequate resources, the challenges of providing care are magnified and compounded by stress, difficult physical labor, out-of-pocket expenses, loneliness and worry. It is no wonder that caregiving, although rewarding in many ways, threatens caregivers’ physical, emotional, mental and financial health.
Many of the difficulties for caregivers boil down to a lack of support. We are in the midst of a critical shortage of direct care workers, which seriously limits the alternatives for even the wealthiest. In addition, there is a dearth of health care professionals with the specialized knowledge and skills needed to provide the counseling and treatments needed to support the physical and emotional needs of those living with dementia, not to mention their caregivers.
Society still too often dismisses the contributions of caregivers as “women’s work” (even though, according to AARP, around 40% of caregivers are men) and ignores the volunteer labor that keeps the long-term care system afloat. About 60% of caregivers, according to the same report, are employed, which results in other challenges. They may experience workplace policies that inadvertently penalize them for being caregivers. Moreover, the federal government has been slow to provide the tangible resources and workplace protections caregivers need. In short, the important and essential work of caregivers remains unnoticed, uncelebrated and largely invisible.
Society still too often dismisses the contributions of caregivers as “women’s work.”
Remedying this complex problem requires a multi-pronged approach, including awareness campaigns that acknowledge and elevate the social value of caregivers, legislation that gives priority to developing essential systems of support, and state and federal funding to increase the skilled health care force.
Tax incentives for employers need to be set up to promote the development of special programs for employed caregivers. Federal and state dollars need to be used to provide health professionals with the skills to support caregivers and manage the symptoms of persons with living with dementia. We also need to earmark more funds for training direct care workers and creating wages and working environments that acknowledge the value of their work.
Federal programs like Medicare need to be adapted to better address the needs of those living with progressive chronic illnesses, and bolster their informal support systems. Critical federal legislation like the Recognize, Assist, Include, Support, & Engage Family Caregivers Act or the Credit for Caregiving Act can help build the infrastructure needed to make resources and tangible support available to caregivers, regardless of economic status, geographic location or race, and relieve their economic burdens. Finally, informal family caregiving needs to be reframed to emphasize its importance both to society and to the U.S. economy.
Bruce Willis’ diagnosis is a tragedy. It does, however, present us with the opportunity to recognize the contributions and needs of informal family caregivers. These unpaid workers provide essential services and prevent the collapse of the long-term care system. They contribute to the lives of those they care for as well as all the rest of us.
Americans don’t like to talk about those in our aging population — what they experience, and how those experiences may affect others around them. We’d prefer to not think about what happens if our minds and bodies start to decline. But caregivers don’t have that luxury. They are the invisible backbone of our society. They can’t look away from this reality — and neither can we.
Linda Phillips
Linda Phillips, Ph.D., RN and FGSA, is a professor of medicine and the director of research and innovation at the Arizona Center on Aging. She also directs the innovations in aging graduate interdisciplinary program at the University of Arizona. She's been a gerontologist for about 40 years, and her research focuses on family caregiving and long-term care for older adults.
Mindy J. Fain
Mindy Fain, M.D., is the Anne and Alden Hart professor of medicine and nursing at the University of Arizona. She is also the co-director of the University of Arizona Center on Aging, and the division chief of general internal medicine, geriatrics and palliative medicine. She is also the associate director for education, care and community research at the University of Arizona Health Sciences Innovations in Aging program.